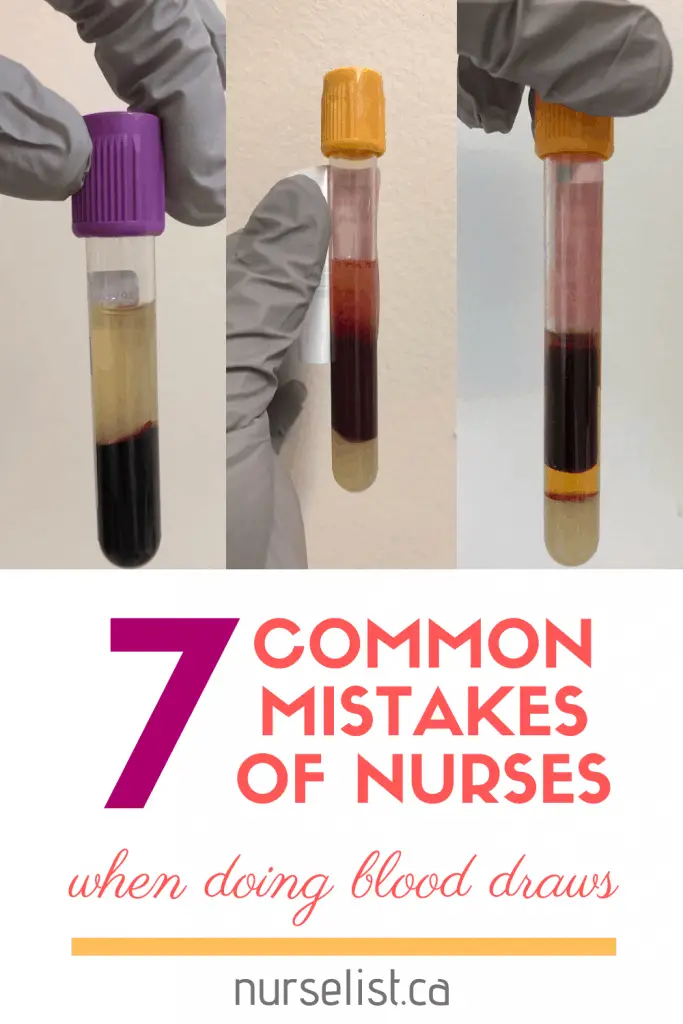
7 Common Mistakes of Nurses When Doing Blood Draws
There was a time in my career when I chose to work as a laboratory assistant and as a phlebotomist. I did blood draws to admitted patients in different units every morning. I also learned how laboratory technicians and medical technologists process blood tubes for different kinds of tests.
As I did my morning rounds of blood draws in different units, I noticed that some nurses are already doing or have already done the blood tests of their patients. And I realized that not all nurses are knowledgeable about the proper techniques in doing blood draws.
But I can’t blame them! Nurses have tons of things to do and blood draws are just one of the many tasks they can quickly do. There are also some important aspects of blood taking that you will only know if you are familiar with how the blood tubes are processed in the laboratory.
So if you don’t want to receive a call from the lab about doing a “recollect” of a certain blood test you just did, learn from the following common mistakes of nurses when doing blood draws:

1. Using a small needle size
Small needle size is often associated with hemolyzed blood sample. As the blood rushes through a small-bore needle, red blood cells can burst because of the pressure. This is known as hemolysis. Laboratories cannot process a hemolyzed blood sample because it yields inaccurate results and machines usually reject it.
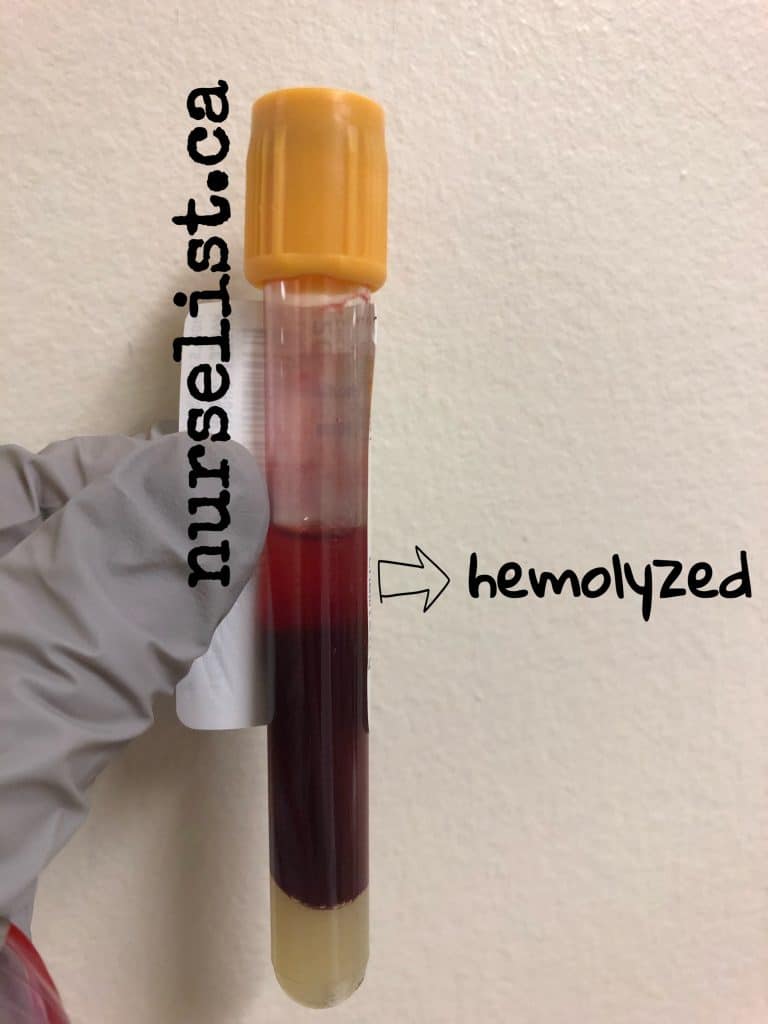
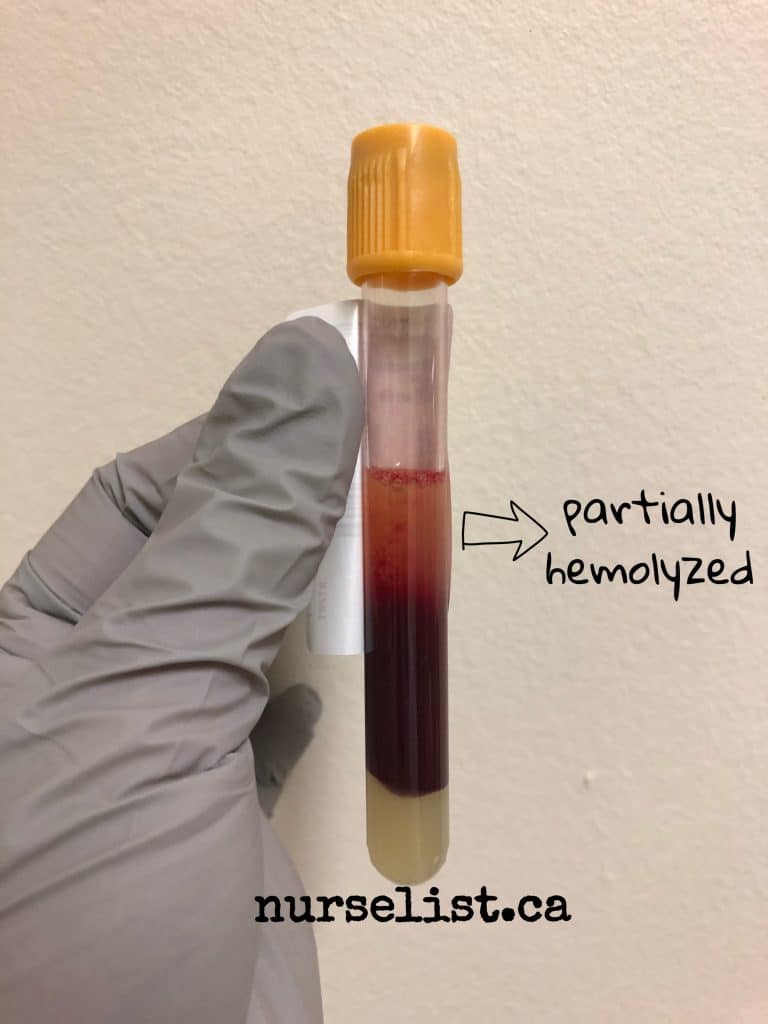
When doing blood draws, I always use 23G (light blue) butterfly needles. If I can see that the patient’s vein is large and I have a lot of tubes to fill, I use a21G (green) butterfly needle or a straight needle. I rarely get a hemolyzed blood sample from these needles. I only use 25G (dark blue) butterfly needle when the patient’s only good vein is a very small one.
2. Improper way of inverting of blood tubes
I noticed that some nurses either overdo or forget doing proper blood tube inversion after collecting blood. It is important to invert blood tubes slowly after blood collection to ensure adequate mixing of blood and additives inside the tube.
Right after the tube has been filled up, gently invert it 8 – 10 times. Don’t shake as this may cause hemolysis.
3. Leaving the tourniquet tight for more than a minute
Leaving the tourniquet tight for more than a minute may also cause hemolysis. When the tourniquet is tight, the pressure building up in the veins may rupture some of the red blood cells flowing through the needle. It is best to leave the tourniquet tight for less than a minute and release it before you completely fill up the last tube of blood.
4. Improper order of draw

Following the proper order of blood draw is important in ensuring accurate results. It prevents contaminating a sensitive tube with the additive from the other tube.
For example, if you will collect blood in a gold (STT) tube first before the light blue tube, the light blue tube will be contaminated with the clot activating additive from the gold tube. The light blue tube is commonly used to measure coagulation factors and if it’s contaminated with the clot activating additive from the gold tube, it will lead to erroneous results.
Another example, if you will collect blood in a lavender tube first before the gold tube, the potassium-based additive of the lavender tube will contaminate the gold tube. This will affect results especially if serum potassium levels are being tested, leading to pseudo hyperkalemia.
5. Insufficient amount of blood sample collected
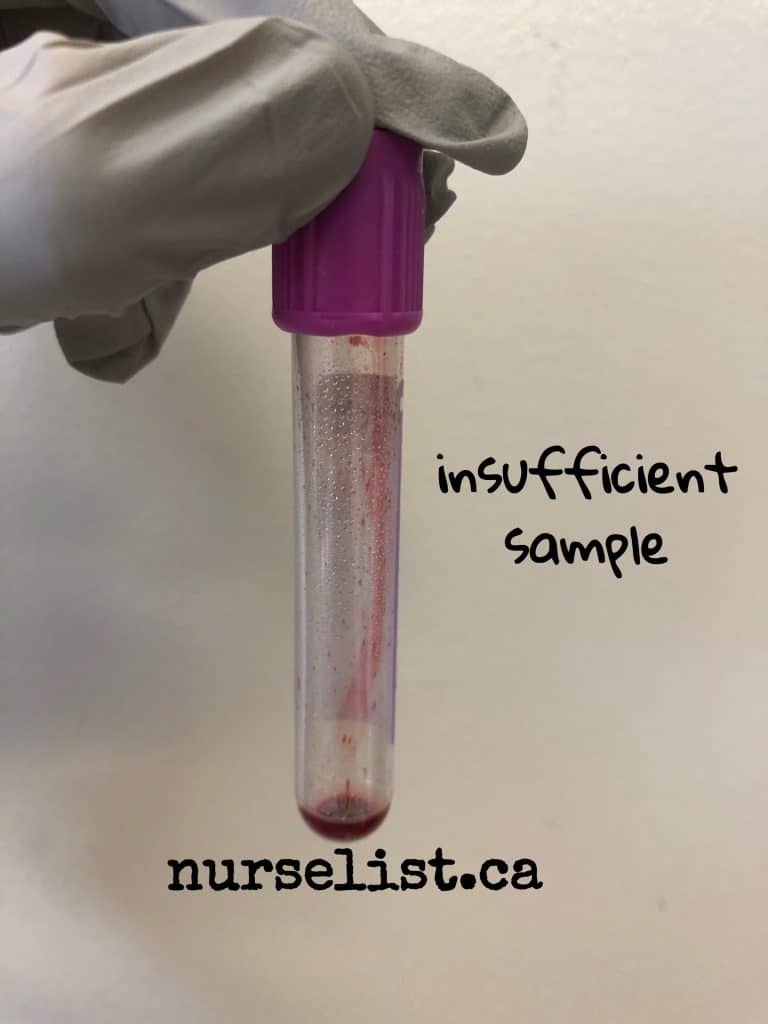
Ideally, blood tubes should be at least half-filled with blood. Laboratories use automated machines for most tests and these machines can only accept blood tubes automatically for processing if it’s half-filled.
However, if it’s really hard to get a blood sample like when the patient is deteriorating, laboratories might accept blood tubes filled with at least half inch to one inch of blood. The automated machines will not accept these blood tubes so the medical technologist will have to process them manually. But take note that this is not acceptable for light blue tubes:
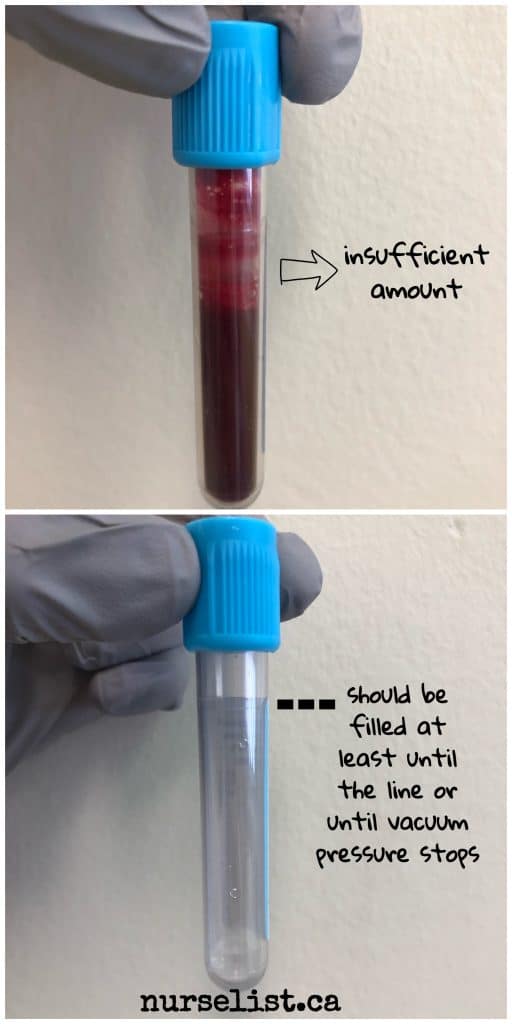
Light blue tubes contain 3.2% buffered sodium citrate. It serves as an anticoagulant. The amount of this additive in each light blue tube is standardized. So this tube should be filled completely with blood until the vacuum pressure from the tube stops or until to the line indicated in the tube. If it’s filled inadequately, it will be rejected by the lab because the additive will be too concentrated in the blood sample collected and it will lead to erroneous results.
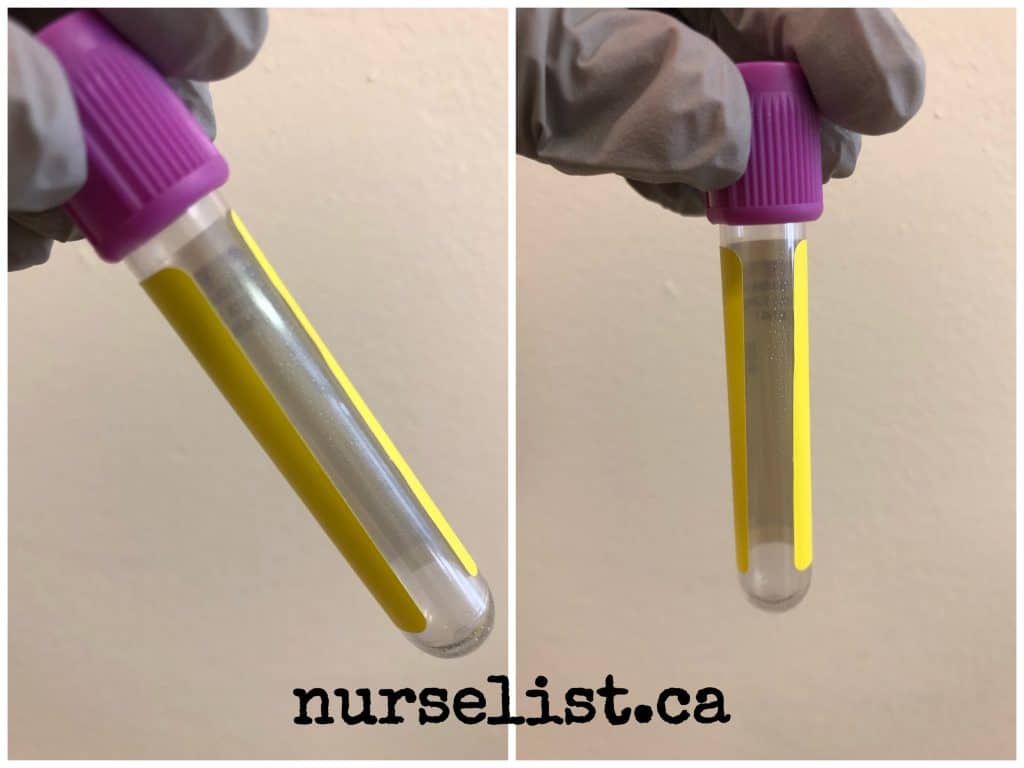
6. Improper labels
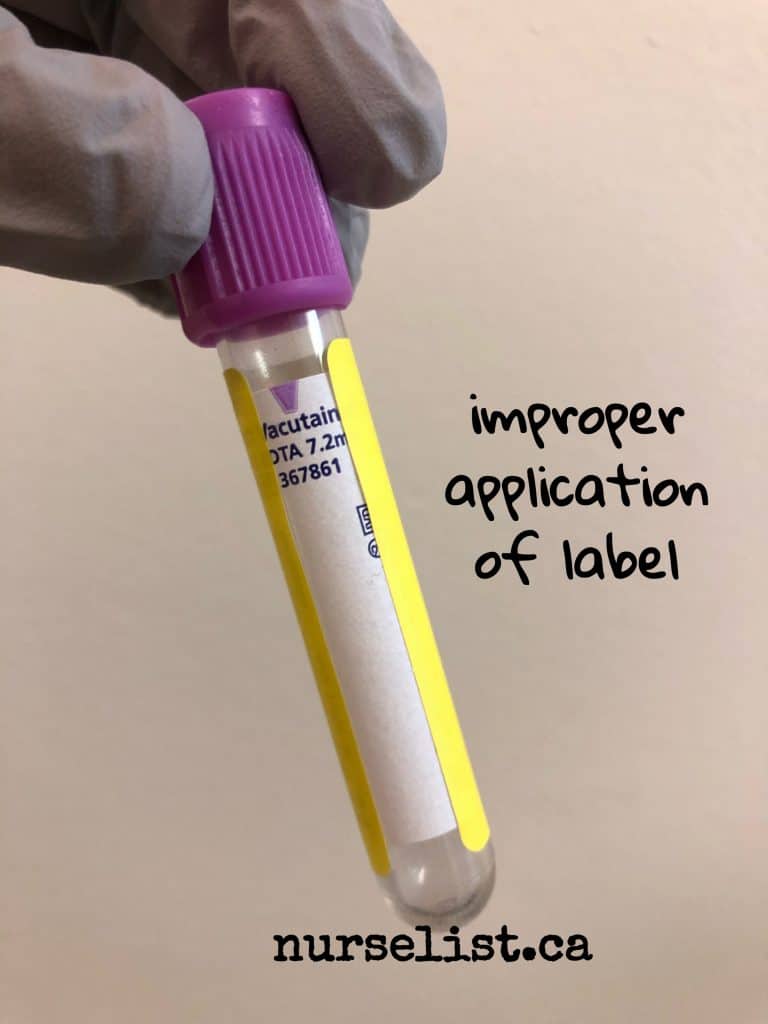
As I mentioned earlier, laboratories use automated machines for processing of common blood tests. Proper application of label plays an important role – the machine cannot scan the tube to verify sufficient blood sample if the tube is entirely covered like in the picture above. You should leave a “window” for the machine to check sample levels like in the picture below. Also, try your best to straighten the label so the scanner in the machine can quickly detect the bar code in the label.
7. Mixing blood samples between different tubes
I once caught a nurse cheating with blood tubes – she opened the top cover of the light blue tube and transferred some of the blood to a gold tube! She said that she did it so she won’t need to poke the patient again because the other test was added late. She was not aware about the different additives in each tube.
Remember that different colors of blood tubes have different additives at controlled concentrations. So even if you transfer blood from a light blue tube to another light blue tube, the result will still be affected as you are also transferring the other tube’s additive.
Never open the top cover of the tubes to transfer blood between tubes. If you got insufficient blood sample, try sending it to the lab for manual processing if the blood level is at least half inch. If you have an additional test for the patient and it requires the same color of tube you just did earlier, just call the lab to manually process the additional test using the blood tube you already did earlier for the other blood test. But if the additional test requires a different color of tube, you definitely need to poke the patient again.

Why would a whole group of lab results (67) come back Critically low CO2’s? Three different nurses drawing all with ample experience?
I had a person take my blood very poor for she had no idea how to insert the needle than try to get blood to flow evenly, she held the tube up ward instead down or level
so the blood would flow, then she tried my right arm same thing but, advantually,she managed to get two tubs an the color light red not dark. For I wasn’t please with her at all this was at the medical centre clinic life labs at 279 wharncliffe road north london,ontario , canada, Just pray that it will be o.k when, the lab test the blood,
sincerely,
helen rose evans